The Gut-Immune Connection in MS and B-Cell Dysregulation
Multiple sclerosis (MS) disrupts the gut-immune connection, but the MS gut-immune restoration protocol offers hope for rebalancing this critical axis. In MS and other autoimmune diseases, the gut microbiome heavily influences immunity through the gut-immune axis. Key bacteria—like Faecalibacterium prausnitzii, Butyricicoccus spp., Roseburia spp., Eubacterium rectale, Coprococcus spp., Akkermansia muciniphila, and Prevotella spp.—produce short-chain fatty acids (SCFAs) such as butyrate, acetate, and propionate, which help maintain immune balance. Yet, in MS patients, these bacteria are often depleted, reducing SCFA levels, weakening regulation, and increasing inflammation. This imbalance can worsen B-cell overactivity, a significant factor in MS progression, as B-cells produce autoantibodies (e.g., against myelin) and activate T-cells. Studies, including a 2016 Nature Communications analysis and a 2021 Cell report, confirm fewer beneficial bacteria in MS patients compared to healthy controls, underscoring the need for gut-immune restoration. For most, MS is the body’s abnormal expression of this disconnect between the gut and immune system. As a doctor and digestion coach of 36 years, gut dysbiosis is a primary issue I help my patients identify and correct. The goal is to bring the body back into balance.
How Depletion Might Increase B-Cell Activity
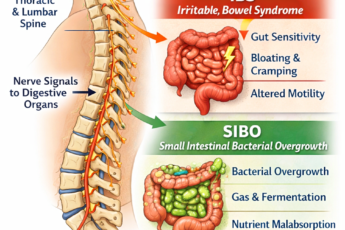
When these helpful bacteria are scarce, disrupting the MS gut-immune restoration process, several problems arise:
- Lower Butyrate Levels: Butyrate usually helps regulatory T-cells (Tregs) suppress harmful immune responses. Without enough butyrate, Tregs weaken, allowing overactive T-helper cells (e.g., Th1/Th17) to stimulate B-cells to produce autoantibodies.
- Gut Dysbiosis: Harmful bacteria, like Enterobacteriaceae, may grow unchecked, releasing toxins such as lipopolysaccharides (LPS). These toxins can activate B-cells, increasing their survival and growth.
- Leaky Gut: A damaged gut barrier allows microbial products to leak into the bloodstream, triggering widespread inflammation and priming B-cells for action.
Together, these issues create a vicious cycle where inflammation and immune dysregulation fuel each other, potentially worsening MS or other B-cell-driven autoimmune diseases.
MS Gut-Immune Restoration Protocol Diet and Lifestyle Strategies
The MS gut-immune restoration protocol boosts these beneficial bacteria and their SCFA production to rebalance the immune system and reduce B-cell overactivity.
1. Increase Dietary Fiber (Prebiotics)
Why It Helps: In the MS gut-immune restoration protocol, beneficial gut bacteria thrive on fermentable fibers, producing SCFAs as a byproduct. Specific fibers, like resistant starch, inulin, fructooligosaccharides (FOS), and pectin, feed bacteria such as Faecalibacterium, Roseburia, and Eubacterium, boosting their numbers and activity.
What to Eat:
Resistant Starch: Found in green bananas, cooked-and-cooled potatoes or rice, green peas, lentils, and chickpeas. Aim for 20-40 grams of total fiber daily.
- Green Peas: One cup (160 g) provides 5-9 g of fiber, including resistant starch (up to 3 g when cooled). A 2020 Nutrients study showed that eating 15 g of pea fiber daily for 4 weeks increased F. prausnitzii and butyrate levels in humans.
- Lentils: One cup (198 g) offers 15-18 g of fiber, including resistant starch (up to 5 g when cooled). A 2019 Journal of Nutrition study found that eating 100 g of lentils daily for 6 weeks raised F. prausnitzii and Roseburia levels by 50%.
- Chickpeas: One cup (164 g) delivers 12-15 g of fiber, including resistant starch (up to 7 g when cooled). A 2022 Gut Microbes study showed that eating 200 g daily increased F. prausnitzii and butyrate by 30-40% in 3 weeks.
Inulin: Found in onions, garlic, leeks, asparagus, and Jerusalem artichokes. Aim for 5-10 g daily. A 2015 Gut study found that taking 10 g of inulin daily doubled F. prausnitzii levels in humans within 2 weeks.
Pectin: Found in apples, citrus fruits, and carrots. This fiber supports Prevotella and Akkermansia. A 2019 Frontiers in Microbiology study showed that pectin increased Akkermansia and SCFA levels in mice, improving gut barrier health.
How to Start:
- Begin daily with 1/4 cup (50-75 g) of legumes, like lentils or chickpeas. Gradually increase to 1 cup (150-200 g) as your body adjusts.
- Add inulin-rich foods, such as 1-2 garlic cloves or half an onion, to meals. For added benefits, include pectin sources, like an apple daily.
- Cook and cool starches (e.g., lentil salad or roasted chickpeas) to boost resistant starch. Soak legumes before cooking to reduce bloating.
Evidence: A 2020 Gut Microbes study showed that a high-fiber diet (30-40 g daily) increased F. prausnitzii and butyrate in healthy adults within weeks. In MS mouse models, fiber improved immune regulation and reduced disease severity (Immunity, 2018), suggesting potential benefits for B-cell activity.
2. Eat Polyphenol-Rich Foods
Why It Helps: For MS gut-immune restoration, polyphenols in colorful fruits, vegetables, and other foods act as prebiotics and anti-inflammatory agents.
They support Akkermansia and butyrate-producing bacteria while reducing inflammation that drives B-cell activation.
What to Eat:
- Berries: Blueberries or blackberries (1 cup daily, ~150 mg polyphenols). A 2021 American Journal of Clinical Nutrition study found that eating 200 g of blueberries daily for 8 weeks increased Akkermansia by 20% and lowered inflammation.
- Dark Chocolate: Choose 70-85% cocoa (30 g daily, ~400 mg polyphenols). A 2018 Frontiers in Immunology study linked cocoa to increased Roseburia and reduced inflammation in rats.
- Green Tea: Drink 1-2 cups daily (~200-400 mg catechins). A 2019 Journal of Nutrition study showed that green tea increased Akkermansia and SCFA production in humans over 4 weeks.
- Olive Oil: Use extra virgin olive oil (2-3 tbsp daily, ~30 mg hydroxytyrosol). A 2020 Nutrients study found that it boosted F. prausnitzii and gut barrier health in people with metabolic syndrome.
How to Start:
Sip green tea mid-morning. Snack on berries or a small piece of dark chocolate (limit to 1 oz to avoid excess sugar). Drizzle olive oil on legumes or vegetables.
Aim for 500-1000 mg of total polyphenols daily. If necessary, track your intake using a food diary.
Evidence: A 2019 human study linked polyphenol-rich diets to increased Akkermansia and reduced inflammation. In MS, polyphenols may directly reduce B-cell activity (Journal of Neuroimmunology, 2017), enhancing gut-focused benefits.
3. Include Fermented Foods (Probiotics)
Why It Helps: Fermented foods contain live microbes that support SCFA-producing bacteria, balance gut pH, and reduce harmful bacteria. This creates a healthy environment for F. prausnitzii and other beneficial species.
What to Eat:
- Kefir: Drink 1 cup daily (~10^9 CFU). A 2021 Cell study showed that kefir increased microbial diversity and butyrate levels in humans after 6 weeks.
- Yogurt: Choose unsweetened yogurt with live cultures (e.g., Lactobacillus, Bifidobacterium), 1 cup daily. A 2019 Nutrients study found that yogurt indirectly boosted Roseburia levels.
- Kimchi or Sauerkraut: Eat 1-2 tbsp daily (~10^8 CFU). A 2020 Food Microbiology study linked kimchi to higher Prevotella and SCFA production in humans.
How to Start:
- Choose unsweetened, live-culture products. Start with 1-2 tbsp of fermented veggies, gradually increasing to 1/2 cup as your body adjusts.
- Pair fermented foods with fiber-rich meals (e.g., sauerkraut with lentils) to enhance benefits.
Evidence: The 2021 Cell study found that fermented foods reduced inflammation by 20-30% in humans, supporting their role in immune regulation relevant to MS.
4. Avoid Gut Disruptors
Why It Helps: Certain factors, like antibiotics, high-fat diets, emulsifiers, sugar, and alcohol, harm SCFA-producing bacteria and promote inflammation.
What to Avoid:
- Antibiotics: A single course can reduce F. prausnitzii by 50% for months (Gut, 2016). Use antibiotics only when necessary, and pair with probiotics afterward.
- High-Fat Diets: Diets high in saturated fats (e.g., >40% of calories) decreased Roseburia in mice (Nature, 2018). Limit saturated fats to less than 10% of your daily intake.
- Emulsifiers: Additives like polysorbate 80 and carboxymethylcellulose (found in processed foods) reduced Akkermansia in humans (Gut, 2020). Check food labels and avoid ultra-processed items.
- Sugar and Alcohol: Excess sugar (>20 g daily) and alcohol increase harmful bacteria in humans (Microbiome, 2019). Limit added sugar to 5-10 g daily and alcohol to 1 drink per week.
How to Start:
- Swap processed snacks for whole foods (e.g., chickpeas instead of chips). Use herbs and spices instead of emulsified sauces.
- After antibiotics, rebuild your gut with 2-4 weeks of high-fiber foods and probiotics (e.g., lentils + kefir).
Evidence: A 2018 Nature study showed that switching to a fiber-rich diet after a high-fat diet restored Roseburia in mice within 3 weeks.
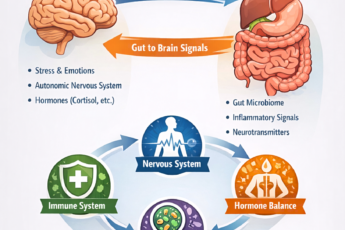
5. Exercise and Manage Stress
Why It Helps: Moderate exercise and stress reduction improve microbial diversity and SCFA production by supporting gut-brain communication and lowering stress hormones, which can harm beneficial bacteria.
What to Do:
- Exercise: Aim for 30-60 minutes of moderate activity, like brisk walking or yoga, 5 days a week. A 2017 Gut study found that this increased F. prausnitzii by 15% in humans after 6 weeks, along with higher butyrate levels.
- Stress Reduction: Practice mindfulness (10-20 minutes daily) or yoga (2-3 sessions weekly). A 2019 Psychosomatic Medicine study showed that mindfulness lowered stress hormones and increased Roseburia in stressed adults over 8 weeks.
How to Start:
- Take a walk after meals to improve gut motility. Try deep breathing or guided meditation before bed.
- Avoid overtraining (e.g., more than 90 minutes of intense exercise daily), as it may increase stress hormones and disrupt your gut.
Evidence: In MS patients, yoga reduced inflammation and improved gut health (Journal of Clinical Neuroscience, 2020), suggesting benefits for overall immune health.
Nutritional Supplements for MS Gut-Immune Restoration
Beyond diet and lifestyle, the MS gut-immune restoration protocol includes supplements to regulate the immune system, including B-cell activity, in autoimmune diseases like MS. These work alongside gut-focused strategies to reduce inflammation and support immune health.
1. Vitamin D
Why It Helps: Vitamin D helps calm overactive B-cells and T-cells, reduces inflammation, and boosts Treg activity.
Evidence: The 2022 VITAL trial (NEJM) showed that taking 2000 IU of vitamin D daily reduced autoimmune disease risk by 22% in over 25,000 adults over 5 years. A 2018 Neurology study found that MS patients with higher vitamin D levels (>40 ng/mL) had fewer relapses and less B-cell activity.
How to Use:
- Take 1000-4000 IU daily, ideally with a fat-containing meal for better absorption. Adjust based on blood tests, aiming for 30-50 ng/mL.
- Test your levels every 6-12 months. To prevent side effects, avoid taking too much (>10,000 IU daily).
Relevance to MS: Vitamin D deficiency is common in MS. Supplementing may help reduce B-cell overactivity indirectly by boosting Tregs.
2. Omega-3 Fatty Acids
Why It Helps: Omega-3s (EPA and DHA) reduce inflammation and alter B-cell activity, potentially lowering harmful immune responses.
Evidence: The VITAL trial showed that taking 1000 mg of omega-3s daily reduced autoimmune risk by 15-18%. A 2020 Journal of Clinical Investigation study found that 2.5 g daily in MS patients lowered inflammation and B-cell activity over 6 months.
How to Use:
- Take 1-2 g of combined 2:1 DHA to EPA daily (from fish oil or algae-based sources). Split doses with meals to avoid a fishy aftertaste.
- Choose high-quality, tested brands to avoid oxidation. If needed, pair with antioxidants (e.g., vitamin E).
Relevance to MS: Higher doses may help in early MS, working alongside gut-based anti-inflammatory effects.
3. Curcumin
Why It Helps: Curcumin, found in turmeric, reduces inflammation by blocking pathways that drive B-cell activation and cytokine production.
Evidence: A 2019 Phytotherapy Research study showed that 500-1000 mg daily (with piperine) improved symptoms in autoimmune diseases over 8 weeks. A 2021 Multiple Sclerosis Journal pilot study found that 1000 mg daily reduced fatigue and inflammation in MS patients, though B-cell effects were not directly measured.
How to Use:
- Take 500-1000 mg daily with 5-10 mg piperine (black pepper extract) or liposomal form for better absorption. Consume with a fatty meal.
- Start with a low dose (250 mg) to check for tolerance. Avoid if you’re on blood thinners, as curcumin may have mild anticoagulant effects.
Relevance to MS: While human data is limited, animal studies suggest curcumin could work with SCFAs to reduce B-cell overactivity.
Potential Benefits
Restoring beneficial bacteria and adding supplements could:
- Boost Immune Regulation: Through gut-immune restoration for MS, higher butyrate and vitamin D levels strengthen Tregs, which help control B-cells (Immunity, 2018).
- Reduce Harmful Antibodies: Lower inflammation from omega-3s and curcumin may decrease B-cell activity (Journal of Autoimmunity, 2019).
- Slow MS Progression: SCFAs and supplements reduced nerve damage in MS animal models (Cell Reports, 2021).
Challenges to Consider
- Individual Differences: Results vary based on your starting gut microbiome, nutrient levels, and disease state.
- Timeframe: Noticeable benefits may take 4-12 weeks of consistent effort.
- Limited Direct Evidence: While animal and observational studies are promising, human trials linking these strategies to B-cell reduction in MS are still limited.
Conclusion: Gut-Immune Restoration for MS
In MS, the loss of SCFA-producing gut bacteria disrupts the gut-immune axis. As a gut health expert, I’m confident that the MS gut-immune restoration protocol can address this imbalance and B-cell overactivity. Digestive coaching tips for restoring these bacteria are through a fiber-rich diet (e.g., green peas, lentils (especially Black Gram [Vigna mungo], chickpeas), polyphenol-rich foods, fermented foods, disruptor avoidance, lifestyle changes, and targeted supplements (vitamin D, omega-3s, curcumin) offers a comprehensive approach to support immune health. While not a cure, this strategy could complement MS treatments by addressing underlying drivers of immune dysfunction.
Recent Updates on Gut Microbiome Research in MS (as of February 21, 2025)
A new study, published on February 21, 2025, in Neurology Neuroimmunology and Neuroinflammation by Yale University and Mayo Clinic, provides fresh insights. Titled “Alterations in Gut Microbiome-Host Relationships After Immune Perturbation in Patients With Multiple Sclerosis,” it analyzed 43 untreated MS patients and 42 healthy controls.
Key findings include:
- Fewer IgA-Coated Bacteria: MS patients had significantly fewer gut bacteria coated with immunoglobulin A (IgA), a marker of immune-microbiome balance. IgA normally regulates gut bacteria, so its reduction may allow harmful bacterial shifts, potentially increasing B-cell activity.
- Effects of B-Cell Depletion Therapy: In 19 patients, 6 months of anti-CD20 therapy (e.g., rituximab) didn’t fully restore IgA coating but shifted bacterial patterns. Some SCFA producers, like F. prausnitzii, showed increased IgA coating, suggesting therapy may partially improve immune-gut balance.
Implications: The study highlights a “fundamental disconnect” in gut-immune interactions in early MS, which may drive B-cell dysregulation. It suggests microbiome changes could serve as biomarkers or treatment targets, though direct effects on B-cell autoantibodies weren’t measured.
This research supports earlier findings on SCFA producer depletion but adds nuance: B-cell depletion therapies may indirectly benefit gut bacteria, yet persistent low IgA coating shows that full gut-immune balance isn’t restored.
COMPLEMENTARY 15-MINUTE CALL
Take your first step toward a renewed sense of well-being. Call today to arrange a complimentary 15-minute consultation.
Let’s discern whether my approach aligns with your needs.
I look forward to connecting with you at 714-639-4360.
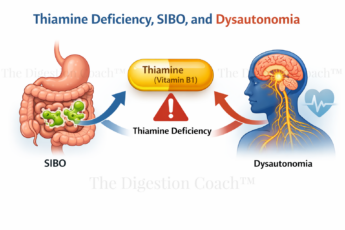
Polyamines and SCFAs + B Vitamins: The Gut-Neurological Link