Table of Contents
- Dysbiosis in CVID Patients
- Gastrointestinal Symptoms and the Microbiome
- Immune Modulation by the Microbiome
- Therapeutic Interventions Supporting the Microbiome and Common Variable Immunodeficiency
- Future Directions
- Conclusion
Common Variable Immunodeficiency (CVID) is a primary immunodeficiency characterized by low immunoglobulin (antibody) levels, resulting in recurrent infections, immune dysregulation, and gastrointestinal complications. Recent research highlights the microbiome’s critical role in the CVID pathophysiology. As a digestion coach, I’m keenly aware that gut dysbiosis, or an imbalance in our microbial community, contributes to systemic and localized inflammation, gastrointestinal symptoms, and immune dysfunction, especially in CVID patients. This article explores the connection between the microbiome and Common Variable Immunodeficiency (CVID), focusing on dysbiosis, immune modulation, and potential therapeutic approaches.
Dysbiosis in CVID Patients
CVID patients often experience significant alterations in their gut microbiota. Studies reveal a reduction in beneficial bacteria, such as Faecalibacterium prausnitzii and Bifidobacterium, known for their anti-inflammatory properties. Conversely, there is an overgrowth of potentially pathogenic bacteria, including Proteobacteria and Enterobacteriaceae. This microbial imbalance exacerbates inflammation and contributes to the chronic immune activation observed in CVID.
Dysbiosis also impacts the gut’s structural integrity, leading to increased intestinal permeability, commonly called “leaky gut.” This allows microbial products like lipopolysaccharides (LPS) to enter the bloodstream, triggering systemic inflammation and potentially worsening autoimmune manifestations prevalent in CVID patients.
Gastrointestinal Symptoms and the Microbiome
A significant proportion of CVID patients report gastrointestinal symptoms, such as diarrhea, bloating, and malabsorption. Dysbiosis is a key factor underlying these issues. The loss of microbial diversity and beneficial bacterial species disrupts normal digestive and absorptive functions, contributing to inflammation and developing conditions resembling inflammatory bowel disease (IBD). My CVID patients and those seeking gut health restoration learn that addressing these microbiome alterations is crucial for managing any or all of the above symptoms.
Immune Modulation by the Microbiome
The microbiome plays a pivotal role in regulating immune function. A healthy microbial ecosystem fosters immune tolerance and prevents excessive inflammation. In CVID, dysbiosis impairs this regulatory mechanism, exacerbating immune dysfunction and chronic inflammation. The interplay between a compromised immune system and an imbalanced microbiome creates a vicious cycle that perpetuates disease progression.
Therapeutic Interventions Supporting the Microbiome and Common Variable Immunodeficiency
Probiotics and Prebiotics
Probiotics, such as Lactobacillus and Bifidobacterium species, are live beneficial bacteria that can help restore microbial balance. They may reduce gut inflammation, improve intestinal barrier function, and alleviate gastrointestinal symptoms. Prebiotics, non-digestible fibers that feed beneficial bacteria, can also promote microbial diversity and enhance the production of short-chain fatty acids (SCFAs) like butyrate, which have anti-inflammatory effects. Combining probiotics and prebiotics (“synbiotics”) offers a promising strategy to support gut health in CVID patients.
Fecal Microbiota Transplantation (FMT)
FMT involves transferring stool from a healthy donor into the gastrointestinal tract of a recipient. This therapy has successfully treated conditions like recurrent Clostridioides difficile infections and holds the potential for restoring microbial diversity in CVID. By introducing a healthy microbial ecosystem, FMT could reduce inflammation and improve gastrointestinal symptoms. However, safety concerns remain, especially in immunocompromised patients, necessitating further research.
Diet
Diet plays a vital role in shaping the microbiome. Anti-inflammatory diets rich in whole foods, fiber, and fermented products can support a healthy microbiome. Eliminating food triggers, such as gluten or dairy, may also help manage gastrointestinal symptoms in CVID patients with sensitivities. Low FODMAP diets, which limit fermentable carbohydrates, may temporarily reduce bloating and discomfort in patients with severe symptoms.
Emerging Therapies
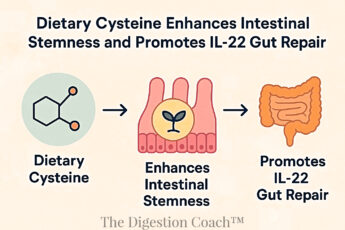
Postbiotics, bioactive compounds produced by probiotics, and microbiome-based pharmaceuticals are emerging areas of interest. These therapies aim to harness the benefits of a healthy microbiome without introducing live bacteria, offering safer alternatives for immunocompromised individuals. Advances in microbiome profiling and personalized medicine may pave the way for tailored interventions based on an individual’s unique microbial composition.
Future Directions
Understanding the relationship between the microbiome and common variable immunodeficiency is still an evolving field. Ongoing research aims to clarify how dysbiosis contributes to immune dysfunction and identify practical, effective, and safe therapies for CVID patients. Personalized approaches targeting the microbiome, coupled with immunoglobulin replacement therapy and other standard treatments, may transform the management of this complex condition.
Conclusion
The microbiome plays a crucial role in the pathogenesis and management of Common Variable Immunodeficiency. Dysbiosis contributes to gastrointestinal symptoms, systemic inflammation, and immune dysregulation in CVID patients. Therapeutic strategies, including probiotics, prebiotics, FMT, dietary interventions, and emerging microbiome-based therapies, offer promising avenues for restoring microbial balance and improving patient outcomes. As research advances, personalized microbiome-targeted therapies may become an integral part of CVID treatment, enhancing quality of life and addressing the multifaceted challenges of this immunodeficiency.
COMPLEMENTARY 15-MINUTE CALL
Take your first step toward a renewed sense of well-being. Call today to arrange a complimentary 15-minute consultation.
Let’s discern whether my approach aligns with your needs.
I look forward to connecting with you at 714-639-4360.