Table of Contents
- Introduction
- My Predisposing Factors
- So What Was the True Cause of My Gastritis?
- Diagnostic Testing
- The True Cause Was H. pylori
- H. pylori Treatment Protocol
- Important Protocol Updates
- Don’t Self Treat
Introduction
First, H. pylori and biofilm are what shaped me into the doctor and digestion coach I am today. I spent hundreds of hours pouring over journals, studying, and emailing researchers to learn all I could about these co-mingling entities. As a result, I have used that same drive to know all I can about the conditions I treat and to build proven protocols that yield predictable results. I hope this post is helpful to you.
H. pylori infection can cause gastritis, ulcers, heartburn, SIBO, anemia, low stomach acid, Insulin resistance, rosacea, anxiety, depression, chronic fatigue, and more. This post will cover everything you need about the original H. pylori treatment protocol. Proven protocols come with years of research and trial and error. Fact: 100% of all H. pylori protocols available today on the web have some or all of their components from this protocol.
“Heartburn, chronic active gastritis, GERD, acid reflux, achlorhydria or H. Pylori – that is the question.” William Shakespeare. Are any of these conditions due to too much stomach acid (hyperchlorhydria)? Not necessarily, and rarely so. I have to admit here that I experienced an acute and severe bout of gastritis when I started my first practice. And yes, it hurt bad! It felt like someone poured a quart of battery acid down my throat; at the same time, I was having a heart attack while licking a brand-new nine-volt battery. I think you get the picture.
Well, to make a long story short, my stress wasn’t going to go away in the next five minutes. I needed to be my own “medical detective” and reverse engineer what was going on based on the condition’s pathophysiology to determine the cause. Knowing the cause and predisposing factors would allow me to apply precise heartburn, H. pylori, chronic active gastritis, GERD, or low stomach HCl treatment.
My Predisposing Factors:
1. Chronic Dehydration – There are different types of mucous cells in the stomach, as well as the small and large intestines, and they are easy sources to supply the body with water when dehydrated. The thinning of the gastric mucosa or destruction of that mucous membrane layer makes the stomach vulnerable to organic acids – hydrochloric or those produced from the fermentation of ingested sugars and purification of ingested proteins. Decreased stomach acid (HCl) due to being locked in a flight-flight mode contributed to the perfect storm for the introduction and/or colonization and/or activation of the dreaded H. pylori bacterium.
2. Zinc Deficiency—I noticed this during a hair mineral analysis. As a singular factor, zinc deficiency would most likely not cause anything overtly noticeable. However, combined with a Helicobacter pylori (H. pylori) infection, the compounding effects created a more severe inflammatory reaction within the gastric lining.
3. One Bourbon, One Scotch, One Beer—Ethanol on its own can cause painful erosion and inflammation of the gastric lining. Still, when combined with zinc (and B1) deficiency, it can compound the degree of inflammation and drastically delay healing.
4. H. pylori or Lack of HCl? After testing, it was confirmed that H. pylori was present. Was my lack of HCl the reason I got H. pylori, or was the H. pylori the cause of the reduced stomach acid? At this point, it didn’t matter because I couldn’t take HCl due to gastritis, and further research showed that the H. pylori bacterium does indeed lower HCl levels (neutralize) in the stomach.
So, to make a long story short, I was up shit-creek without a paddle, and I was also missing the canoe.
So What Was the True Cause of My Gastritis?
#1, #2, #3, and #4 all played their individual parts in my condition. A little more on #4 – Achlorhydria (lack of stomach HCl) or H. pylori bacteria: This is the, what came first, chicken or the egg dilemma. Did my lack of stomach acid allow the H. pylori a safe haven to take up residence, or did the H. pylori infection cause the lack of stomach acid? Both are possible, and both allow the other to exist and create a painful condition called atrophic gastritis. This is exactly what I had, and, I am sure, a little erosive gastritis as well.
Diagnostic Testing
After some diagnostic testing: allopathic (traditional medicine), which included Diagnostic Solutions GI-MAP (GI-MAP | GI Microbial Assay Plus w/ H. pylori Antigen and Virulence Factors – $425) and energetic testing (Applied Kinesiology & Contact Reflex Analysis), I now knew what was going on, what caused it and what to do to get it completely under control. It was confirmed I did have Helicobacter pylori – H. pylori for short.
Urea Breath Test vs Stool Antigen Testing – The Prefered Method of Testing
The H. pylori Urea Breath Test (30C UBT) is a sensitive and specific method for the non-invasive detection of H pylori infection. Still, gastric bacterial overgrowth may lead to a false positive diagnosis. Patients with low to no hydrochloric stomach acid can present with many urease-positive bacteria other than H. pylori. The vigorous urease activity may be responsible for false positive results of an H. pylori Urea Breath Test in patients with suspected H. pylori infection.
References:
Urease-positive bacteria other than Helicobacter pylori in human gastric juice and mucosa.
Gastric bacterial overgrowth is a cause of false positive diagnosis of Helicobacter pylori infection using 13C urea breath test.
The True Cause Was H. pylori.
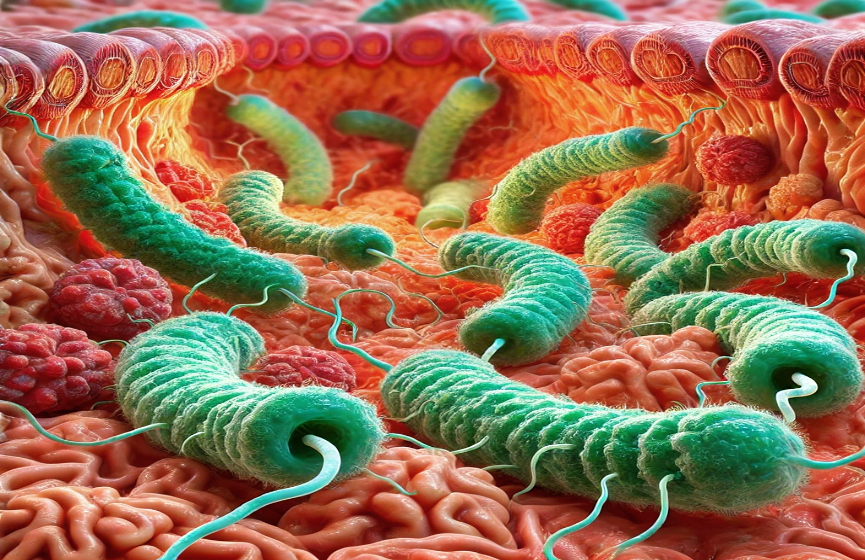
One of our oldest companions is a microbe called Helicobacter pylori, or just H. pylori. It has been colonizing our stomachs and co-evolving with us for the past 50,000 – 100,000 years. H. pylori is a spiral-shaped gram-negative bacterium identified in 1979[1].
H. pylori, in those infected, can thrive in their gastric epithelium and in the thin layer of overlying mucus that protects the stomach wall from the stomach’s hydrochloric acid. This unique niche is hostile to nearly all other microbes. One mechanism by which the bacterium does this is by producing urease in abundance. It is reported that urease functions in H. pylori infection to neutralize gastric acid by producing ammonia (NH3). Enhanced production of NH3 also may facilitate the formation of NH3-derived compounds, such as monochloramine, which shows cytotoxic effects on host cells. Enhancement of bacterial motility and inhibition of phagocytic clearance of bacteria were also reported as functions of urease.[6]
About half of the world’s population house H. pylori in their stomach and are unphased by it. However, in 10-15 percent of those infected, the microbes cause peptic ulcers and chronic active gastritis. In an unluckier bunch, about 2%, H. pylori is a causative agent for gastric (stomach) cancer and mucosa-associated lymphoid tissue lymphoma[2]. It has also been shown to be associated with extra-gastric diseases, such as Sjogren’s syndrome (affecting salivary glands), Hashimoto’s thyroiditis (affecting the thyroid gland), and infections in the small intestine related to Campylobacter jejuni. It has also been shown to be associated with extra-gastric diseases, such as unexplained refractory iron deficiency anemia and idiopathic thrombocytopenic purpura[3-5].
“Everybody with Helicobacter does have inflammation or some irritation in the lining of the stomach, and because it lasts your whole life, it gradually builds up. This means Helicobacter needs to be treated in people, even if they do not feel unwell.” Professor Barry Marshall. Emeritus Professor Robin Warren and Professor Barry Marshall received the Nobel Prize in 2005 for discovering Helicobacter pylori.
References:
- Pajares JM, Gisbert JP. Helicobacter pylori: its discovery and relevance for medicine. Rev Esp Enferm Dig 2006; 98: 770-785
- Sari YS, Sander E, Erkan E, Tunali V. Endoscopic diagnoses and CLO test results in 9239 cases, prevalence of Helicobacter pylori in Istanbul, Turkey. J Gastroenterol Hepatol 2007; 22:1706-1711
- Bohr UR, Annibale B, Franceschi F, Roccarina D, Gasbarrini A. Extragastric manifestations of Helicobacter pylori infection — other Helicobacters. Helicobacter 2007; 12 Suppl 1: 45-53
- Franceschi F, Roccarina D, Gasbarrini A. Extragastric manifestations of Helicobacter pylori infection. Minerva Med 2006;97: 39-45
- Franceschi F, Gasbarrini A. Helicobacter pylori, and extragastric diseases. Best Pract Res Clin Gastroenterol 2007; 21: 325-334
- Hideo Kuwahara et al., Helicobacter pylori Urease Suppresses Bactericidal Activity of Peroxynitrite via Carbon Dioxide Production. Infect Immun. 2000 Aug; 68(8): 4378–4383.
H. pylori Treatment Protocol Evolution
You must become an in-office or distance patient to receive additional protocol information or digestive coaching for H. pylori, SIBO, biofilm, or related GI health issues. I want to help you, and I can create a protocol tailored to your situation. Please call for a complimentary 15-minute consultation to see if we are a good fit: 714-639-4360
The Original H. pylori Pre-treatment protocol
First, I took antacids (over-the-counter – Zantac OTC, an H2 blocker) to increase the susceptibility of the H. pylori to treatment (eradication), lessen the need for H. pylori to defend itself so vigorously, and to allow my gastric mucosa a chance to heal. At least, that was what I was thinking at the time. Note: H. pylori forms protective bacterial colonies called biofilm, which comprises a protective, extracellular polysaccharide shield. This protective shield is a defensive barrier against stomach hydrochloric acid and other substances, like antibiotics. Being a complex matrix of proteins and carbohydrates, which are probably interdependent, the H. pylori biofilm could offer a protective haven for the survival of this gastric bacterial pathogen in the extra-gastric environments (Proteomannans in Biofilm of Helicobacter pylori ATCC 43504). As well as Candida albicans and other bacteria.
The Current H. pylori pre-treatment protocol
The current protocol consists of a personalized, 30-day BIOFILM PROTOCOL and Gut Restoration Protocol. Since H. pylori bacteria can produce biofilm and are becoming more immune to conventional antibiotics daily, through experience, I have found it helpful to weaken its outer defenses before the Marines (natural antimicrobial agents and antibiotics) are sent in.
The Original H. pylori Treatment protocol
My personal H. pylori bomb consisted of Monolaurin (lauric acid) or Lauricidin – also see coconut oil, which is 50% lauric acid by weight) and H-PLR (K-32) (Supports bacterial elimination) from Apex Energetics. I also juiced 1/4 cabbage every day (cabbage contains S-Methylmethionine, known as Vitamin U, a great healer of ulcers and gastritis). After 4 weeks of my protocol, I felt like a new man! After 8 weeks (stool test), I re-checked myself and was free of the foreign invaders; a breath test confirmed the same.
The Current H. pylori Treatment protocol
This protocol comprises the Prevpac, Omeclamox®-Pak, or Pylera pharmaceutical regime and a personalized combination of natural antimicrobial agents. Below are the products I’m currently pulling from to create a customized protocol. Having (1) the correct biofilm and (2) H. pylori protocol is just as crucial as having (3) the proper therapeutic dosage for the products used. To the degree that the balance of the three is off is to the degree that the entire protocol may fail. This is why it is always best to have a qualified coach and never self-treat.
- Pylopass (no longer available) Pyloguard by Microbiome Labs is available now – Learn more about Pylopass – “Pylopass Eliminates H. pylori with Confidence.”
- Black Seed Oil (Nigella Sativa)
- H-PLR and/or Bio-HPF and/or Berbemycin.
- S. boulardii
- Nutricillin
- Monolaurin – Monolaurin has been shown to inactive many forms of bacteria and viruses protected by an outer lipid membrane.
- Bladderwrack
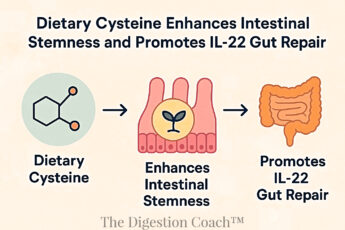
- NAC
- 50:1 Cranberry Extract
- Gastro Comfort and/or Gastrazyme
- InterFase Plus or InterFase
- Triple or Quadruple Antibiotic Therapy
- A More Streamlined Version Of The Personalized Biofilm Protocol
- A Personalized Version Of My Health Restoration Shake
- Lifestyle Modification: Certain dietary restrictions and additions may be warranted and are determined on a case-by-case basis. The two required for everyone are: avoid all cow’s milk and gluten-containing products.
Below are the products I don’t use or recommend as part of a natural H. pylori protocol. These are not bad products in themselves; I’ve just found them to be weak or ineffective.
- Mastic Gum
- Matula tea
- Manuka Honey
As of September 2009, I’ve added Klaire Labs—InterFase Plus (use under a doctor’s supervision or recommendation as it contains the chelating agent EDTA) or InterFase to my H. pylori treatment protocol. InterFase Plus or InterFase is now an essential and mandatory protocol component. It supports the eradication of biofilm, a significant advancement to the protocol.
Understanding biofilm basics and its relevance in GI disorders is extremely important. Please follow any biofilm link to learn more about it, especially the biofilm protocol. Again, please do not self-treat.
Prevention and Healing
Lastly, I needed to keep the H. pylori bacteria from returning and keep the healing process moving forward. I took pancreatic enzymes w/HCl* and plant-based with each meal, as well as zinc** and L-carnosine**. Gastro Comfort from Now Foods has both. Mastic gum***, TheraAloe (No longer available), chlorella and/or spirulina, a daily broad-spectrum probiotic (VSL#3 or Probiotic-10 from Now Foods), NAC, psyllium husk fiber and tons of distilled water, for 6 weeks. I was now better than before my first symptom.
Overall, it was a learning experience that has made me a better doctor and a more diligent medical detective.
FYI: Gastritis is not a single condition; it is a series of conditions that all share stomach lining inflammation as a common symptom. Gastritis, most often, is caused by prolonged use of non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or aspirin, chronic dehydration, drinking too much alcohol, or infection such as Helicobacter pylori bacteria (H. pylori). It may also occur after major surgery, severe infections, trauma injury burns, or severe infections. Some diseases, such as pernicious (B12 deficiency) anemia, autoimmune diseases, and chronic bile reflux, can also cause gastritis.
*Microscopy studies of the motility of H. pylori in gastric mucin at acidic and neutral pH in the absence of urea show that the bacteria swim freely at high (alkaline – achlorhydria) pH and are strongly constrained at low (acidic) pH. Also, H. Pylori, through enzyme reactions, promotes increased ammonia production, which raises the pH of its environment – allowing it to move more freely.
**A combination of zinc and L-carnosine has been shown to prevent gross visible damage to gastric mucosa caused by ethanol ingestion. This combination also acts as a potent antioxidant, benefiting the gastric mucosa. Polaprezinc, a mucosal protective agent, in combination with lansoprazole, amoxicillin, and clarithromycin, increases the cure rate of Helicobacter pylori infection
***There is conflicting data on whether mastic gum kills H. pylori effectively in vivo (live human trials). Killing it in a test tube or mice is one thing, but I am interested in living human beings. Evidence shows that it aids in healing the gastric mucosa, possessing anti-inflammatory properties. I used it for healing rather than as an agent to kill the H. pylori bacteria. Note: some studies have shown that mastic gum kills H. pylori. The problem is that it is less than 30% of the trial groups. So it works in about one out of every three that try it as a primary treatment (at 500 mg 3x/day).
Important Protocol Updates
PLEASE READ This Updated, Update 19 August 2014. The original update was on August 08, 2013. Why H. pylori Infections Are So Hard To Treat? – As a doctor and digestion coach, I have been helping patients with H. pylori, a biofilm-producing bacteria, for almost 7 years. In the beginning, eradicating this bug was very easy, in my opinion. As time progressed, I noticed that the same protocol I had been using was becoming less and less effective – on first-timers, not re-treatments. There are now H. pylori strains that are multiple drug-resistant. Medically, there is no real explanation for this. Energetically, there is a perfect explanation, for me anyway, based on the research done by Rupert Sheldrake, Ph.D. on Morphic Fields and Morphic Resonance. Please read about his theory for further clarification.
Because of this new shift in loss of effectiveness, in some patients, I have had to use more than one round of products or add more products to the protocol. The result has always been eradication, but it’s now taking more effort to achieve this result. Also, many people are contacting me and letting me know that they have undergone triple and quadruple therapies to no avail. In my mind, this proves that biofilm and the bacteria that create them are learning to defend themselves more effectively. They are adapting and mutating genetically to survive. Good for them and bad for us.
My theory is that with the introduction of hundreds of blogs, chat rooms, and websites devoted to H. pylori and biofilm, more and more people are self-treating. This self-treating does not kill H. pylori or eliminate the biofilm; conversely, it makes them both stronger by strengthening the biofilm defense. Every time a bacteria that produces a biofilm is unsuccessfully treated, it becomes more resistant to the following protocol. Combined with the Morphic Fields theory, it’s no wonder that H. pylori and biofilm eradication are becoming harder and harder to achieve. The point of all of this is that there are still effective treatment options available; it may just take a little more time and/or more products, allopathic (Prevpac or Pylera) and/or natural, to get to the desired result – H. pylori and biofilm eradication.
Don’t Self Treat
Lastly, as a gut health specialist, I am not against self-treating per se. The issue is that the information on the internet on biofilm and H. pylori treatment protocols is not comprehensive or transparent enough for the layperson to be their own doctor or to successfully self-treat. I have always advocated and promoted that if you want to get better with or at something, you need a coach who is an expert in that field or subject. There are times and places where self-help is good, but biofilm and H. pylori treatment are not one of them. This is just my opinion.
Follow this link to access all of the data within my original H. pylori post on www.advancedhealing.com, which was unsuitable for this revised post. The post above is a revised version that is protocol-based only. The linked page will have H. pylori news, articles, and original post updates.
COMPLEMENTARY 15-MINUTE CALL
Take your first step toward a renewed sense of well-being. Call today to arrange a complimentary 15-minute consultation.
Let’s discern whether my approach aligns with your needs.
I look forward to connecting with you at 714-639-4360.