Table of Contents
- A Common Misconception About Digestive Health
- What the Study Investigated
- Biological Mechanisms Explained in Plain English
- Clinical Interpretation
- Systems Biology Integration
- Why This Matters for Long-Term Health and Healthspan
- Practical Implications
- Grand Conclusion
- Educational FAQs
A Common Misconception About Digestive Health
Many people assume chronic digestive symptoms begin and end in the gut. If bloating, irregular bowel habits, or abdominal discomfort persist, the instinct is to look only at food choices, stomach acid, or intestinal bacteria. Yet modern research increasingly shows that digestion does not operate in isolation. The gut functions as part of a larger communication network involving the brain, immune system, and nervous system. Importantly, evidence indicates that gut–brain axis dysfunction is a cause of many persistent symptoms. More and more, experts are recognising the impact of gut–brain axis dysfunction on digestive health and overall well-being. In this article, we’ll explore what gut–brain axis dysfunction is and how it can affect your health.
A recent narrative review published in Cureus highlights an important shift in understanding: many functional gastrointestinal disorders may reflect disrupted signaling within the gut–brain axis rather than structural problems within the digestive tract itself. These disrupted signals are a hallmark of gut–brain axis dysfunction.
What the Study Investigated
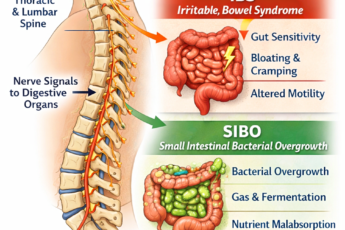
The review examined how bidirectional communication between the brain and gastrointestinal system influences digestive function. Researchers explored evidence showing that functional gastrointestinal disorders — such as irritable bowel syndrome (IBS), functional constipation, and chronic bloating — often occur without visible disease but still produce significant symptoms.
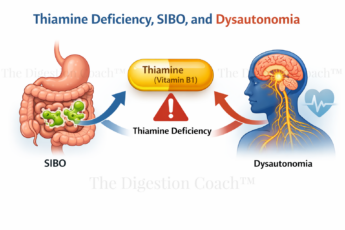
The authors evaluated how stress physiology, nervous system regulation, microbial signaling, and immune responses interact to influence gut motility, sensitivity, and inflammation. Rather than focusing on a single pathway, the study emphasized the modulation of multiple systems simultaneously. Furthermore, gut–brain axis dysfunction can disrupt these interconnected systems.
Biological Mechanisms Explained in Plain English
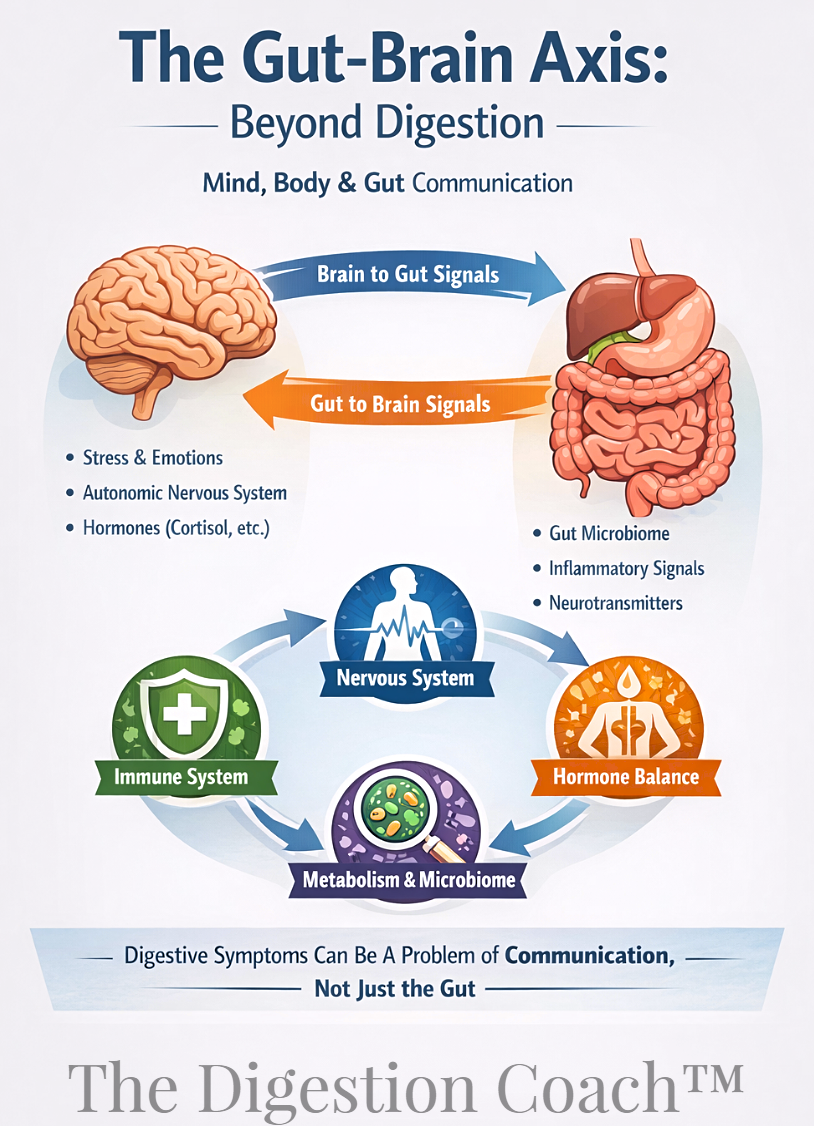
The gut and brain are constantly communicating through nerves, hormones, immune signals, and microbial metabolites. This network is commonly called the gut–brain axis.
Signals traveling from the brain to the gut influence digestion through autonomic nervous system activity, stress hormone release, and changes in intestinal movement and secretion. At the same time, signals traveling from the gut to the brain include microbial byproducts, inflammatory signaling molecules, vagus nerve communication, and neurotransmitter precursors produced in the intestine.
When communication remains balanced, digestion feels predictable. When signaling becomes dysregulated — often due to chronic stress or sleep disruption — symptoms can develop even when the digestive tract appears structurally normal. In short, gut–brain axis dysfunction often explains how otherwise normal tests can lead to uncomfortable symptoms.
From a Clinical Perspective…
From a clinical perspective, these findings help explain why patients with chronic digestive complaints frequently report overlapping symptoms such as anxiety, poor sleep, fatigue, or heightened stress sensitivity. Many individuals notice their digestive symptoms fluctuate more with stress levels than with specific foods.
This also clarifies why dietary interventions alone sometimes provide incomplete relief. When nervous system signaling remains dysregulated, the gut continues receiving inconsistent regulatory input regardless of dietary adjustments.
Systems Biology Integration
The gut–brain axis illustrates how multiple physiological systems operate as an integrated network.
- The nervous system regulates motility and sensitivity.
- The immune system influences inflammation and barrier integrity.
- The microbiome produces metabolites affecting digestion and mood.
- The endocrine system modulates stress hormones that alter gut function.
- The brain interprets and amplifies sensory signals originating in the intestine.
A disturbance in any one component can influence all others, explaining why digestive disorders often coexist with mood changes, fatigue, or immune dysregulation.
Why This Matters for Long-Term Health and Healthspan
Understanding digestion through a regulatory lens shifts the focus from symptom suppression toward maintaining physiological resilience. Chronic dysregulation of the gut–brain axis may contribute not only to digestive discomfort but also to systemic inflammation, metabolic stress, and reduced stress tolerance over time.
When communication between systems becomes inefficient, the body expends more energy maintaining balance, which may influence long-term healthspan.
Practical Implications (Educational Only)
This research encourages a broader understanding of digestive health. Instead of viewing symptoms solely as local gastrointestinal problems, it may be more accurate to consider how stress physiology, sleep patterns, immune signaling, and nervous system regulation influence digestion.
Recognizing that fluctuating symptoms can reflect regulatory changes rather than structural disease often helps patients better understand their experiences.
Grand Conclusion
Modern research increasingly supports a shift in how we understand digestive disorders. The gut is not an isolated organ but part of an adaptive communication network linking brain, immune, and metabolic systems. When signaling across this network becomes disrupted, symptoms emerge even in the absence of visible disease. Therefore, gut–brain axis dysfunction is a crucial factor in many unexplained symptoms.
Viewing digestive health through the lens of regulation rather than dysfunction alone allows many chronic symptoms to make physiological sense and highlights the importance of integrated system balance.
Educational FAQs
What is the gut–brain axis?
It is the communication system connecting the digestive tract and brain through nerves, hormones, immune signals, and microbial activity.
Why can digestive symptoms occur with normal test results?
Functional disorders often involve signaling and regulation problems rather than structural damage detectable on imaging or lab tests.
Can stress really affect digestion?
Yes. Stress hormones and nervous system activity directly influence gut movement, sensitivity, and secretion.
Why do digestive symptoms often occur with anxiety or poor sleep?
The same regulatory systems influence both brain function and gastrointestinal activity.
Does this mean digestive disorders are “all in the head”?
No. Symptoms are real physiological responses caused by changes in communication between body systems.
At Advanced Healing Center in Orange, CA, Dr. Marcus Ettinger focuses on identifying root-cause physiology behind chronic digestive, metabolic, and inflammatory conditions.
Evans C, Kalman D. Addressing GI Health Through the Bidirectional Modulation of the Gut-Brain Axis With Herbal Extracts: A Narrative Review. Cureus. 2024;16(8):e66698. DOI: 10.7759/cureus.66698







Leave a Comment