Introduction: Could Carbohydrate Maldigestion Be Causing Your Gut Issues?
If you’ve ever felt bloated, gassy, or had diarrhea after eating certain foods, you might be dealing with carbohydrate maldigestion. This common yet often overlooked condition can mimic irritable bowel syndrome (IBS) and wreak havoc on your gut health. In a recent clinical review published in The American Journal of Gastroenterology (April 2025), experts dive into the science of carbohydrate maldigestion, its causes, and how to manage it effectively. Whether you suspect lactose intolerance, sucrose intolerance, or another issue, this guide breaks down everything you need to know in simple terms. Let’s explore what carbohydrate maldigestion is, its symptoms, and practical solutions to feel better fast.
Carbohydrate maldigestion happens when your body struggles to break down complex carbs (like lactose or sucrose) into simple sugars for absorption. When these carbs reach your colon undigested, gut bacteria ferment them, producing gas and causing symptoms like:
- Bloating
- Diarrhea
- Abdominal pain
- Flatulence
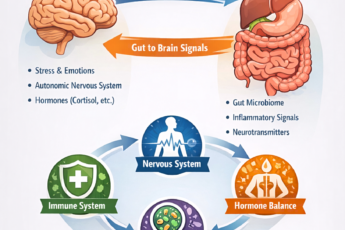
This condition is especially common in individuals with disorders of gut-brain interaction (DGBI), such as IBS, and can be triggered by specific sugars like lactose, sucrose, fructose, or FODMAPs.
Key Fact: Not everyone with maldigestion experiences symptoms. When symptoms occur, it’s called carbohydrate intolerance.
Common Causes of Carbohydrate Maldigestion
- Congenital Lactase Deficiency: A rare genetic condition causing lactose intolerance from birth.
- Congenital Sucrase-Isomaltase Deficiency (CSID): The most common inherited deficiency, affecting sucrose and starch digestion. CSID Diet Page
- Other Deficiencies: Rare issues like maltase-glucoamylase or trehalase deficiency.
Secondary Causes
- Gut Damage: Conditions such as celiac disease, Crohn’s disease, or infections can reduce enzyme production.
- Pancreatic Issues: Insufficiency or surgery affecting digestion.
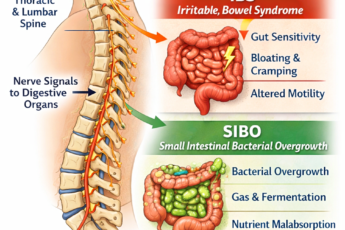
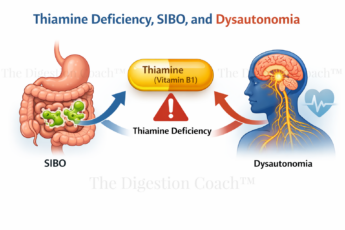
- SIBO or Rapid Transit: Small intestinal bacterial overgrowth or fast gut motility can interfere with absorption.
Did You Know? Secondary causes are often temporary and improve when the underlying condition is treated.
Symptoms: When Carbs Cause Trouble
The symptoms of carbohydrate maldigestion are similar to IBS, making it tricky to diagnose. Common signs include:
- Diarrhea: Especially after eating trigger foods like dairy (lactose) or sugary fruits (fructose).
- Bloating and Gas: Caused by bacterial fermentation in the colon.
- Abdominal Pain: Often worse after meals.
- Nausea or Vomiting: More common with severe cases.
For example, CSID may cause lifelong, frequent symptoms after consuming sucrose-rich foods (e.g., table sugar, fruits), while lactose intolerance typically occurs after dairy consumption.
Pro Tip: Keep a food diary to track symptoms and identify trigger foods.
Diagnosing Carbohydrate Maldigestion
Diagnosing carbohydrate maldigestion requires a mix of clinical history, tests, and dietary response. Here are the primary methods:
1. Hydrogen Breath Testing
- How It Works: You consume a test carb (e.g., lactose, sucrose, fructose), and breath samples measure hydrogen levels. A rise of ≥20 ppm indicates maldigestion.
- Pros: Non-invasive and widely available.
- Cons: False positives from SIBO or rapid gut transit; requires strict pre-test prep (e.g., fasting, avoiding antibiotics).
2. Duodenal Disaccharidase Assay
- How It Works: A biopsy from your small intestine measures enzyme activity (e.g., lactase, sucrase).
- Pros: Gold standard for confirming enzyme deficiencies.
- Cons: Invasive and depends on proper sample handling.
3. Genetic Testing
- How It Works: Identifies mutations in genes like those for lactase or sucrase-isomaltase.
- Pros: Confirms genetic causes.
- Cons: Not routine due to variable symptom expression.
Important: A positive test doesn’t always mean symptoms. As a digestion specialist, I will assess if symptoms align with test results.
Managing Carbohydrate Maldigestion: Practical Solutions
Good news: Carbohydrate maldigestion is manageable with the right approach. Here’s how:
Dietary Modifications
- Goal: Reduce trigger carbs while keeping your diet as flexible as possible to avoid nutritional gaps.
- Lactose Intolerance: Limit dairy to 12-15 g/day (e.g., small amounts of milk with meals). Try lactose-free products.
- CSID: Start with a sucrose-free diet, then reduce starches if needed. Foods like avocados, broccoli, and almonds are low in sucrose and starch.
- Fructose Intolerance: Keep fructose <10 g/day and balance with glucose-rich foods (e.g., bananas, berries).
- Work with a Digestion Coach: A professional like me can guide you through elimination and reintroduction phases, ensuring a balanced diet.
Enzyme Replacement Therapy
Enzyme therapy can help! For CSID, sacrosidase is a game-changer, letting you enjoy a less restricted diet. For lactose issues, try lactase supplements. Unfortunately, there’s no enzyme fix for fructose intolerance yet, but xylose isomerase shows promise.
Digestion Coach Pro Tip: Always consult a doctor before starting supplements.
Lifestyle Tips
- Track Symptoms: Use a food diary to pinpoint triggers.
- Stay Hydrated: Diarrhea can dehydrate you, so drink plenty of water.
- Manage Stress: Anxiety can worsen gut symptoms, so try relaxation techniques like yoga or meditation.
The IBS Connection: Why It Matters
Carbohydrate maldigestion is often mistaken for IBS due to overlapping symptoms. Studies show:
- High Prevalence: Up to 9% of kids and 7% of adults with IBS-like symptoms have sucrase or maltase deficiencies.
- Genetic Link: Mutations in the sucrase-isomaltase gene are associated with an increased risk of irritable bowel syndrome (IBS).
- Diet Challenges: Low FODMAP diets may not be suitable for individuals with CSID, but a sucrose- and starch-reduced diet can be beneficial.
If you’ve been diagnosed with IBS but still struggle, ask your doctor about testing for carbohydrate maldigestion.
Conclusion: Take Control of Your Gut Health
Carbohydrate maldigestion doesn’t have to rule your life. By understanding your triggers, getting the proper tests, and working with a dietitian, you can manage symptoms and enjoy a more comfortable, flexible diet. Whether it’s lactose, sucrose, or fructose causing trouble, solutions such as dietary adjustments and enzyme therapy can make a significant difference.
Ready to feel better? Please give me a call for a complimentary 15-minute consultation to discuss your situation and determine if we’re a good fit.
COMPLIMENTARY 15-MINUTE CALL
Take your first step toward a renewed sense of well-being. Call today to arrange a complimentary 15-minute consultation.
Let’s discern whether my approach aligns with your needs.
I look forward to connecting with you at 714-639-4360.