Introduction
The human digestive system, while fundamentally the same across genders, operates differently between men and women due to hormonal, anatomical, and physiological factors. These differences contribute to the unique way that digestive problems in women manifest, making their experiences distinct from those of men. By understanding these variations, healthcare providers can better diagnose and treat conditions that disproportionately affect women, such as irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD). Moreover, exploring the reasons behind these gender-specific digestive problems in women helps shed light on the underlying causes and possible interventions for improving their overall gastrointestinal (GI) health.
Hormonal Influence and Pain Sensitivity
Research indicates that women are more prone to chronic pain, including abdominal pain, compared to men. This disparity is partly due to hormonal fluctuations during the menstrual cycle, driven by estrogen and progesterone levels. These hormones affect not only pain perception but also GI motility and sensitivity. For example, digestive problems in women, such as bloating and abdominal cramping, often worsen during certain phases of the menstrual cycle. This connection underscores the importance of considering hormonal influences when addressing GI issues in women.
Prevalence of Gastrointestinal Disorders
Irritable Bowel Syndrome (IBS)
IBS is 2 to 6 times more common in women than men. This condition stems from a complex interplay between gut nerve signaling, brain-gut communication, and stress responses. Emotional stress often exacerbates IBS symptoms, which include diarrhea, constipation, bloating, and abdominal pain. These symptoms typically improve after bowel movements but can significantly impact a woman’s quality of life. Addressing stress management is, therefore, a critical component in treating IBS, a key contributor to digestive problems in women.
Inflammatory Bowel Disease (IBD)
IBD, which includes Crohn’s disease and ulcerative colitis, occurs twice as frequently in women as in men. Symptoms such as chronic diarrhea, rectal bleeding, weight loss, and anemia often require tailored treatment plans. Understanding how hormonal cycles influence inflammation can enhance the management of IBD in women and improve long-term outcomes.
Unique Sensory and Functional Differences
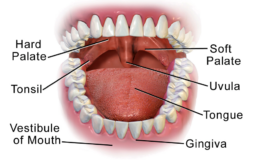
Women’s heightened sensory perception extends to their GI systems. According to taste researcher Linda Bartoshuk, women are more likely to be “supertasters,” experiencing sweet and bitter flavors more intensely. Similarly, the GI tract in women is more sensitive to pressure and irritation. This heightened sensitivity contributes to the unique presentation of digestive problems in women, including a greater prevalence of conditions such as gastritis and acid reflux.
Esophagus and Stomach Functionality
The lower esophageal sphincter (LES) in women is stronger than in men, reducing the likelihood of acid reflux. However, women produce less stomach acid (HCl), which slows digestion and may reduce the effectiveness of certain medications that require an acidic environment. Additionally, women are more susceptible to H. pylori infections, leading to an increased risk of gastritis and ulcers. These factors highlight the need to tailor medical approaches to address the specific digestive problems of women.
Gastric Emptying and Nausea
Women experience slower gastric emptying, contributing to symptoms such as bloating and nausea. Gastroparesis, or delayed gastric emptying, is more common in women and is often associated with diabetes, thyroid dysfunction, or prior surgeries. Proper diagnosis and treatment, including dietary modifications, are essential to managing this condition.
Gallbladder and Liver Differences
Women are more likely to develop gallstones due to slower gallbladder emptying and the impact of estrogen on bile composition. Gallstones are a significant cause of digestive problems in women, particularly during pregnancy or hormonal therapy. Addressing these issues requires a comprehensive approach that considers hormonal influences and dietary factors.
The Role of Stress and Leaky Gut
Chronic stress is a well-known contributor to GI dysfunction, disproportionately affecting women. Stress-induced “leaky gut” increases intestinal permeability, which can trigger autoimmune responses. Conditions like Hashimoto’s thyroiditis are more common in women and have been linked to digestive issues. Testing for markers such as zonulin can help identify leaky gut as a factor in digestive problems in women and guide effective treatment strategies.
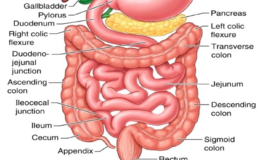
Large Intestine and Bowel Function
Women’s colons are anatomically longer and more complex than men’s, contributing to a higher prevalence of constipation and bloating. Hormonal fluctuations during perimenopause further exacerbate these issues, slowing intestinal motility. Additionally, women’s weaker anal sphincters and shorter anal canals can lead to episodes of incontinence, making bowel control another area of concern in digestive problems in women.
Conclusion
A unique combination of hormonal, anatomical, and physiological factors influences digestive problems in women. From IBS and IBD to gastritis and gallstones, these issues require gender-specific approaches to diagnosis and treatment. By acknowledging these differences, healthcare providers can improve outcomes for women experiencing GI disorders. Further research into these distinctions will pave the way for more effective and personalized care, ensuring that digestive problems in women are addressed with the attention they deserve.






Leave a Comment